Visual Symptoms in Postural Tachycardia Syndrome
A prolific group of neurologists in Bern team up with biomedical engineers for a case-controlled study of posture-dependent visual symptoms in POTS.

New Research
Rodriguez, B., Pantano, L., Nef, T., Müri, R. M. & Z’Graggen, W. J. Visual symptoms in postural tachycardia syndrome: An investigation of position-dependent visual exploration. European Journal of Neurology 32, e16507 (2025).
https://onlinelibrary.wiley.com/doi/full/10.1111/ene.16507
- Published on the 18 September 2024
- Case-control
- 15 patients, 15 controls
- Evidence for Pathology
- Researchers from the University of Bern
- No conflicts of interest, no declaration of funding
Headlines
- The POTS patients were all female, and all classified as having "neuropathic POTS."
- Patients showed a reduction in peripheral visual exploration and increased blurred vision when tilted to 60\( ^{\circ} \) compared to lying down (supine) and controls.
- Controls did not show any position-dependent changes in visual exploration.
- Patients showed increased pupil diameter during tilt–a classic sign of stress–but controls did not.
- Since the automatic visual functions controlled by the brainstem were unaffected by POTS, it's likely the reported visual changes in POTS are caused by a normal visual response to an abnormal adrenergic state.
This study gives an interesting and valuable insight into the pathology of visual symptoms in POTS, suggesting they are a normal visual-neurological response to abnormal autonomic conditions (hyperadrenergic state).
Review
All of the patients in this study had "neuropathic POTS," a diagnosis made after examinations and testing explained in the neurologists' previous research,[1] specifically:
- medical history,
- physical and neurological examination,
- cardiovascular autonomic function testing,
- thermoregulatory sweat test and/or quantitative testing of sudomotor axon reflexes,
- measurement of plasma norepinephrine concentrations,
- determination of autoantibodies against G-protein-coupled receptors,
- and in some cases skin biopsies.
This work-up must make the majority of neurology departments blush. Anyway, this POTS group were all women, and had supine heart rates of 68.87±12.00 bpm (mean±SD) and 99.80±17.06 bpm when tilted to 60\( ^{\circ} \). It would be nice to have two or three men in there, and I'm sure they wouldn't be short of volunteers!
Controls were recruited via flyering the University of Bern campus. No pregnant or breast feeding candidates were accepted, and those selected were aged 18-60. Additional exclusion criteria for control subjects included untreated hypertension, vasovagal syncope in medical history and intake of vasoactive medication. Both groups were asked to stop all vasoactive or psychoactive medication five half-lives prior to testing.
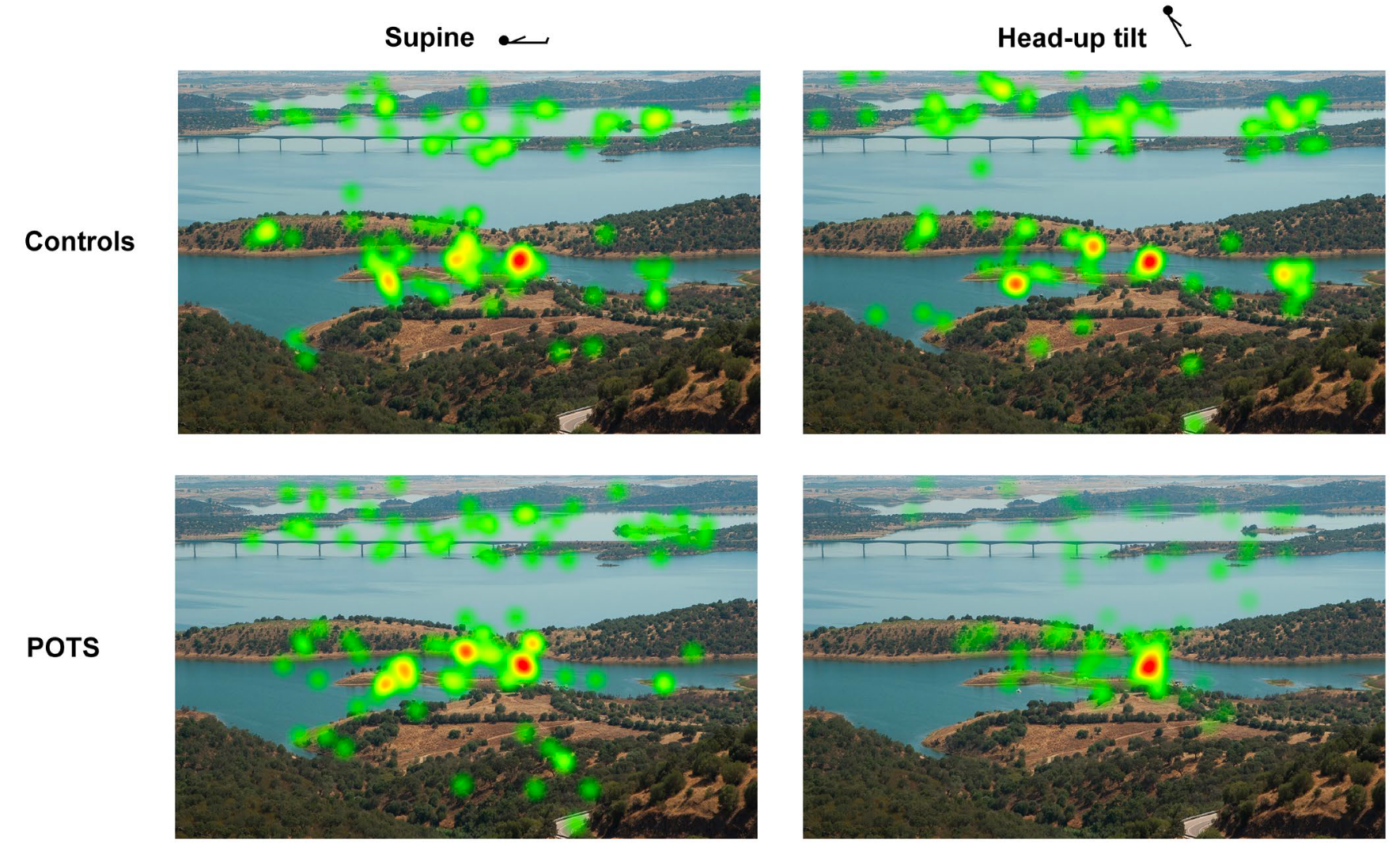
A screen was fitted to the tilt table and the participants were shown images like those above (without the heat maps, which indicated where the eye is focussed) in supine and tilted positions. Measurements of eye movement and pupil size were recorded alongside autonomic data like beat-to-beat blood pressure (BP) and heart rate (HR), intermittent brachial BP and HR, and data from a 3-lead electrocardiogram.
POTS patients showed a reduction in peripheral visual exploration and increased blurred vision when tilted to 60\( ^{\circ} \) compared to lying down (supine) and controls. They also showed increased pupil diameter during tilt.
Additionally the "saccade main sequence," which is the correlation of peak velocity and amplitude of involuntary rapid eye movements, was anlysed during the visual exploration tasks. No difference was found between POTS and controls in either position. This indicates "intact function of the paramedian pontine reticular formation in the brainstem," which is to say that the mechanics of the automatic visual scanning movements are not pathological in POTS.
Furthermore, "the efferent part of the pupillary light reflex, assessed by the constriction velocity, was normal in POTS." So, it seems like the visual functions controlled by the brainstem are not pathological in POTS.
POTS is often reported as "a disorder of the autonomic nervous system." Indeed, these results suggest visual symptoms are not caused by a pathological visual nervous system itself, rather that the visual system is responding normally to an abnormal adrenergic state. The authors discuss this and note that their results are "supported by several eye tracking studies that were conducted with healthy individuals under an artificially generated stress situation and that found similar phenomena to the results of the present study."
So, in conclusion, we have more evidence that innapropriate adrenergic states cause pathology in POTS. In particular there is evidence here of blurred vision and tunnel-vision-like tendencies measured as reduced peripheral exploration. Additionally, there is evidence against compromised visual pathways in the brain. Are blurring and tunnel vision the only visual symptoms in POTS? Sign up for free and you can comment below!
Thank you to all of the patients, families, doctors, healthcare professionals, scientists, engineers and everyone else working to understand and improve the lives of people with POTS. Please join and subscribe.